Intervention Endoscopy
Interventional Endoscopy is an advanced endoscopic technique that not only diagnoses but also treats various gastrointestinal (GI), hepatobiliary, and pancreatic conditions. Unlike traditional diagnostic endoscopy, interventional endoscopy includes therapeutic procedures that eliminate the need for invasive surgery.
Indications for Interventional Endoscopy
Gastrointestinal Conditions:
- Removal of polyps or tumors.
- Treatment of bleeding ulcers or varices.
- Closure of fistulas or perforations.
- Management of achalasia or strictures (narrowing).
Hepatobiliary and Pancreatic Conditions:
- Bile duct stone removal.
- Stenting for bile or pancreatic duct obstructions.
- Treatment of bile leaks.
Other Therapeutic Uses:
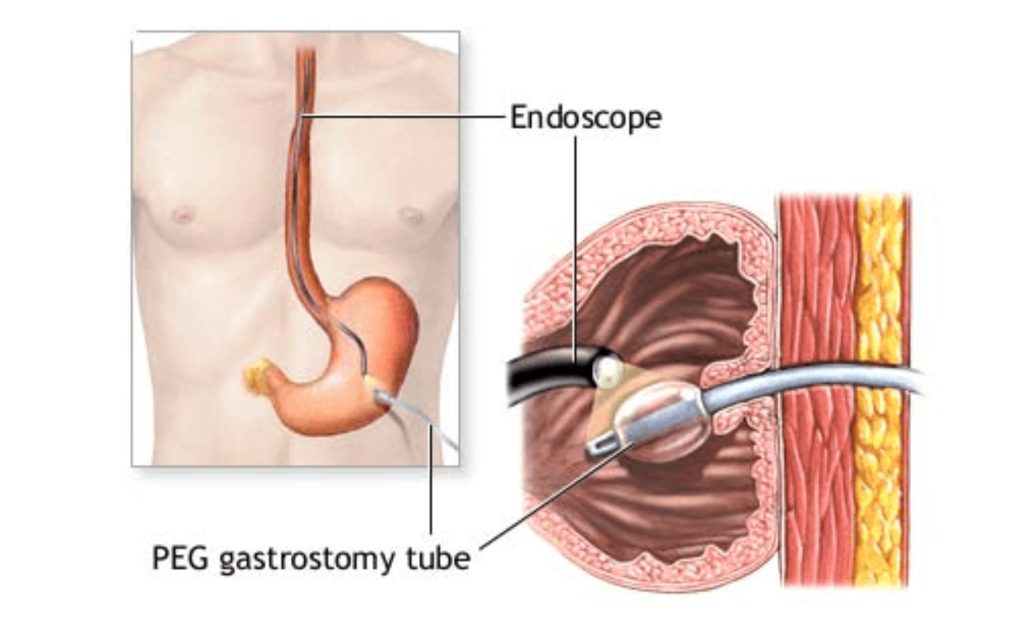
- Placement of feeding tubes (PEG or PEJ).
- Endoscopic mucosal resection (EMR) or submucosal dissection (ESD) for early cancer removal.
Procedure Steps
Preparation:
- Fasting: Patients should not eat or drink for 6–8 hours before the procedure.
- Medication Adjustment: Anticoagulants and certain medications may need to be paused.
- Imaging: Pre-procedure imaging (e.g., CT or MRI) may be performed to guide the intervention.
Sedation or Anesthesia:
- Conscious sedation, deep sedation, or general anesthesia is administered to ensure patient comfort.
Insertion of the Endoscope:
- The patient is positioned based on the procedure (e.g., lying on the side or back).
- A specialized endoscope equipped with tools for therapeutic intervention is gently introduced through the mouth or anus.
Intervention Techniques:
- Hemostasis for Bleeding:
- Clips, cautery, or injection of hemostatic agents are used to stop GI bleeding.
- Polyp and Tumor Removal:
- EMR: The lesion is lifted with a solution, then resected with a snare.
- ESD: More complex tumors are dissected from deeper layers of the GI tract.
- Stone Removal:
- Stones in the bile or pancreatic ducts are extracted using baskets or balloons.
- Stricture Dilation:
- Narrowed areas are widened using balloons or bougies.
- Stent Placement:
- Metal or plastic stents are placed to relieve obstructions in the bile duct, esophagus, or colon.
- Closure of Defects:
- Perforations, leaks, or fistulas are closed using clips, sutures, or stents.
- Hemostasis for Bleeding:
Completion:
- The endoscope and all instruments are carefully withdrawn.
- The procedure duration varies depending on the complexity, typically 30–120 minutes.
Post-Procedure Care
Recovery:
- Patients are monitored in the recovery area until sedation effects wear off.
- Mild discomfort, such as bloating or a sore throat, may occur.
Diet:
- A light diet is recommended initially, progressing to normal meals as tolerated.
Follow-Up:
- Immediate findings are discussed with the patient.
- Further treatment, if required, is planned based on pathology or outcomes.
Dr. Masfique Ahmed Bhuiyan
- MBBS (DMC), BCS (Health)
- FCPS (Surgery), F.A.C.S, F.M.A.S
- Assistant Professor
- Surgical Gastroenterology
- Laparoscopic and Intervention Endoscopic Surgeon
- Dhaka Medical College Hospital, Dhaka.
Opening Hours
- Eden Multi-Care Hospital (Pvt) Ltd
- Visiting hours: Saturday, Monday and Tuesday from 3 pm to 8 pm.